In modern society the prevalence of insomnia and the use of sleep medication have increased substantially over the years. Prior to the coronavirus pandemic, approximately one in ten adults had chronic insomnia (Roth, 2003) and the prevalence was one in three for those visiting their general physician (Swapna,2016). According to several published studies the pandemic has further severely disrupted sleep raising these rates to more than fifty per cent of people which has led in turn to more and more patients seeking treatment from practitioners of Traditional Chinese Medicine for their difficulty sleeping. The sleep difficulties are not only in people recovering from COVID-19, but in the far larger number of people whose lives have been turned upside down due to fear of becoming ill and dying as well as social isolation and stress due to lockdowns.
In my experience, the crux of modern chronic disease according to TCM is often Liver-Spleen Disharmony (i.e. Liver depression qi stagnation + Spleen qi xu) due to our lifestyle, diet and ways of living in the world. These factors are even more present due to the stress of the current pandemic that is aggravating or causing these patterns to be more apparent. From this starting point as practitioners we can search to see if any of the other five depressions (yu) have developed and are present; if the Liver-Spleen disharmony is causing/or is the result of blood/yin xu and also determine if harassment by heat evils (depressive, deficiency and/or phlegm) co-exist as well. All of these factors may cause insomnia by themselves or when combined.
One common scenario met with chronic insomnia (including COVID-somnia) in clinical practice (especially in women) is a patient presenting with dual vacuity (xu deficiency) of the Heart and Spleen as the primary imbalance that needs to be addressed. This underlying diagnosis directs the practitioner to the use of Restore the Spleen Decoction (gui pi tang) – 归脾汤. This article will explore the use of this commonly prescribed formula and how it may be adapted and applied to the modern insomniac.
Gui Pi Tang
The standard formula Gui Pi Tang is one of the most widely employed in China for the treatment of insomnia (Yeung, 2012). The functions of the formula are to boost the qi and supplement the blood, fortify the Spleen and
nourish the Heart. This formula is indicated for both 1) Heart (blood)/Spleen (qi) dual vacuity (deficiency) and 2) Spleen not gathering/holding the blood. According to formula textbooks Gui Pi Tang is indicated to address the main signs & symptoms of these two indications:
1) Heart palpitations, poor memory, insomnia, night sweats, vacuity heat (i.e., feverishness), diminished appetite, bodily fatigue, a faded yellow facial color, a pale, fat tongue with thin, white coating, and a fine, relaxed/retarded or fine, weak pulse
2) Hemafecia, uterine bleeding, early periods, excessive menstruation but pale colored blood or dribbling and dripping which will not stop, or abnormal vaginal discharge.
The origin of Gui Pi Tang – 归脾汤is first attributed to the book Ji Sheng Fang (Formulas to Aid the Living) (Dharmananda, 2002) that was published in 1253 CE during the middle of the Jin-Yuan medical reform period (1127-1368). This book was written by Yan Yonghe who was a well-respected doctor from the Song Dynasty. Yan was recognized as a younger contemporary of Li Dongyuan (aka Li Gao) who emphasized the supplementation of the Spleen and Stomach and wrote the book Pi Wei Lun (Treatise on Spleen and Stomach. Published 1249). Yan Yonghe, like Li Gao, emphasized the importance of the Spleen and Stomach in the cause of and treatment of
diseases and this is apparent in his composition of his formula Gui Pi Tang. The character Gui means to return or restore and therefore this decoction is used to restore/return the vitality (i.e. qi) of the Spleen [pi].
Composition**:
ren shen (Panax ginseng C.A. Mey.) 6g
(most times replaced with dang shen (Codonopsis pilosula (FRANCH.) 9-18g
huang qi (Astragalus membranaceus (FISCH.) 9-30g
bai zhu (Atractylodes macrocephala KOIDZ.) 9-20g
da zao (Ziziphus jujube MILL.) 9g
gan cao (Glycyrrhiza uralensis RISCH.) 3-9g
fu shen or fu ling (Poria cocos (SCHW.)WOLF) 9g
long yan rou (Dimocarpus longan (LOUR.)STEUD.) 9g
suan zao ren (Ziziphus spinosa HU) 9-18g
mu xiang (Aucklandia lappa Decne.) 6-9g
dang gui (Angelica sinensis (OLIV.)DIELS) 9g
yuan zhi (Polygala tenuifolia WILLD.) 6-9g
sheng jiang raw (Zingiber officinale (WILLD.)ROSC.) 3g (often I remove this ingredient to make room for other ingredients and not all of my patients have raw ginger at home)
The original formula did not contain dang gui and yuan zhi. The addition of these two medicinals were first recorded approximately 300 years after the original formula in a Ming Dynasty book focused on treating women’s disorders called Jiaozhu Furen Liangfang (Revised Fine Formulas for Women).
** These are the common dosages and modifications that I use in my clinical practice depending on the patient’s clinical presentation**
Chinese medicine and sleep
According to traditional Chinese medicine (TCM), the three main organs involved in insomnia are the Heart, Liver and Spleen. Although the Heart is involved in all cases, its disturbance tends to be secondary, meaning it is only negatively affected after other organs have become diseased. The Heart stores the shen (mind, spirit) and is considered the emperor of the body-mind in TCM. Shen is nothing other than the accumulation of qi in the Heart, which is constructed and nourished by blood and essence. Healthy sleep should be sound and restful and not disturbed by excessive or scary dreams. Normal dreaming (that does not disrupt sleep) shows that the shen is
relatively quiet and calm. If the shen becomes disturbed – either due to malnourishment or harassment by pathological qi – it may not be able to sink back down and inwards calmly and quietly as it should. In that case either the person cannot fall asleep or, if they do fall asleep, they are unable to stay asleep for a normal length of time.
Malnourishment & Non-construction
As mentioned above, shen is the accumulation of qi in the Heart, which is constructed and nourished by blood and essence. The main organs involved in the construction and nourishment of the shen are the Heart and Spleen. Blood is a tangible substance that is born of unsubstantial qi. When qi is deficient and has no strength to perform its engendering and transformation functions, blood deficiency can occur. Blood is the mother of qi; hence, when blood is deficient, qi is deprived of support, resulting in qi deficiency. For this reason, treatments addressing either of these deficiencies should support the other as well. Qi and blood deficiency will lead to the Heart being deprived of proper nourishment. In this case, the shen will become disturbed and unable to remain still and calm during sleep.
In clinical practice, it is common for patients with insomnia to present with Heart (blood) – Spleen (qi) dual vacuity as part of their clinical presentation. This is especially apparent in females who have a tendency to a weaker Spleen due to menstruation, childbirth and breastfeeding.
Reliable indicators of Spleen qi vacuity in clinic include:
• Fatigue
• Cold hands (and nose)
• Loose stools
• Loss of strength in the hands and feet
• Swollen tongue
• Abdominal distension (after meals)
• Orthostatic hypotension i.e. dizziness on standing or
change of position
• Bruising easily
The Register of Chinese Herbal Medicine Journal. Vol 18, N˚1
Within the formula Gui Pi Tang, ren shen (or dang shen), huang qi, bai zhu, gan cao, sheng jiang, and da zao are all sweet and warm, supplement the Spleen, and boost the qi.
Once a practitioner confirms Spleen qi deficiency is present, they should check to see if the person also presents with the following patterns caused by this imbalance:
• Liver Depression Qi Stagnation
• Food Stagnation
• Phlegm-Dampness
• Blood Stasis
• Blood Deficiency (Heart and/or Liver) >> Yin Deficiency >> Deficiency Heat
• Kidney Yang deficiency
Blood deficiency
Sleep involves the sinking of the yang qi of the Heart downwards into the interior to be enfolded by yin. If the Heart-shen is not properly nourished it can lead to a person being unable to fall or stay asleep for a sufficient period of time. Difficulty falling asleep (but once asleep staying asleep) is often thought of as a sign of blood deficiency, whereas waking frequently during the night feeling hot (with possible sweating) is classified as a symptom of Yin Deficiency.
The main pathomechanism of blood deficiency in clinical practice is hypofunction of the Spleen and Stomach. Since the blood is governed by the Heart, stored by the Liver and produced and managed by the Spleen, blood deficiency is intimately related to these organs. In clinical practice to achieve better outcomes it is important to distinguish whether the patient is presenting with a pattern of Heart or Liver blood deficiency, or both. The signs and symptoms associated with these patterns are as follows:
• Heart blood deficiency: Heart palpitations or fearful throbbing (zheng chong), dizziness, pale face, lips and tongue, fine pulse and symptoms of disquieted heart shen such as heart vexation, insomnia, profuse dreaming and forgetfulness.
• Liver blood vacuity: Dizziness, tinnitus, dry eyes, loss of visual acuity, night blindness, tingling and numbness of the limbs, hypertonicity of the sinews, twitching cramps or tremor of muscles; soft, thin or pale, ridged or brittle nails, scanty, delayed or menses with pale scanty menstrual blood or no menses, parasomnias or behavioural abnormalities during sleep including sleepwalking
and -talking (which indicate the possible involvement of the hun [ethereal soul]).
Gui Pi Tang contains ingredients that nourish both Heart and Liver blood with more emphasis on Heart blood. Dang Gui is sweet, acrid and warm with the ability to nourish the liver, engenders Heart blood and also quicken the blood. Fu Ling, suan zao ren, and long yan rou are sweet and level or neutral in nature. When combined in this formula they nourish the Heart and quiet the spirit. In addition, fu ling also transforms dampness and fortifies the Spleen.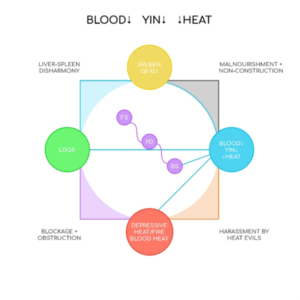
When blood deficiency is present then the practitioner should be aware the following patterns will be more likely:
• Spleen Qi Deficiency
• Liver Depression Qi Stagnation
• Blood Stasis
• Yin Deficiency >> Deficiency Heat
Robert Helmer, RAc, RTCMP, Lakeside Health, Salmon. Arm BC
Book with Rob HERE.



